Contents
- 0.1 RelatedPosts
- 0.2 Unmasking the Killers: BBC Africa Eye’s ‘Blood Parliament’ Exposes Fatal Shootings During Kenya Finance Bill Protests
- 0.3 Pope Francis’ Legacy: A Pope for the Poor, the Marginalized, and Global Unity
- 0.4 Trump – Zelensky Spat: Is the Age of Modest Pretense Gone?
- 1 Mpox: A Comprehensive Overview and the WHO’s Global Health Emergency Declaration
- 2 W.H.O Declares Mpox a Global Health Emergency
- 3 Global Spread of Mpox:
- 4 The Relationship Between Mpox and Smallpox
- 5 Mpox Mutation and New Variants
- 6 Mpox Health Risks and Global Impact
- 7 Public Health Responses and Capacity to Manage Mpox
- 8 Sign up for Mania Africa
- 9 Final Thoughts
In a significant move, the World Health Organization (WHO) has declared Mpox (formerly known as Monkeypox) a global health emergency of international concern. This decision underscores the severity and quick spread of the current Mpox outbreak, prompting nations to intensify their efforts to control and mitigate the disease. This article delves into the critical aspects of Mpox, including its symptoms and transmission, and provides critical facts about the virus.
Mpox: A Comprehensive Overview and the WHO’s Global Health Emergency Declaration
What is Mpox?
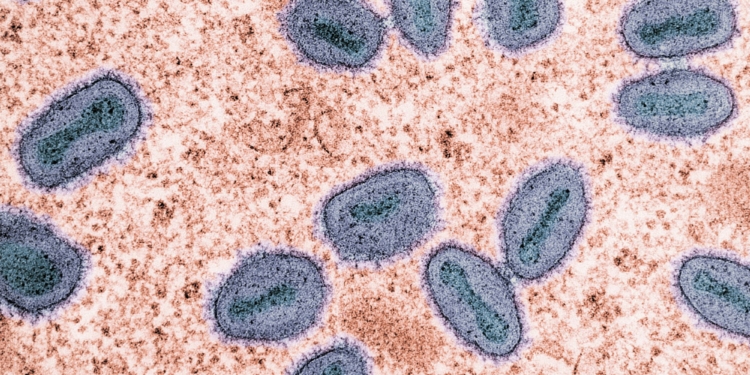
Mpox is a viral zoonotic disease caused by the monkeypox virus, closely related to the variola virus which causes smallpox. It is a viral infection that can spread between people, occasionally from the environment via objects and surfaces touched by an infected person, and from animals to humans in certain settings.
Mpox was first identified in humans in 1970 in the Democratic Republic of Congo (DRC) and has since been reported in various Central and West African countries. The disease manifests with symptoms similar to, but milder than, smallpox, including fever, rash, and swollen lymph nodes.
Mpox Symptoms, Diagnosis, & Prognosis: Critical Facts You Need to Know
Symptoms of Mpox
Mpox typically presents with an incubation period of 5 to 21 days and can cause a range of symptoms, including a rash that could last 2–4 weeks. Common symptoms include fever, headache, muscle aches, back pain, low energy, and swollen glands. The rash looks like blisters or sores and can appear on the face, palms, soles, groin, genitals, and anal regions, as well as inside the mouth, throat, anus, rectum, vagina, or eyes.
Inflammation of the rectum (proctitis) and genitals may occur, causing severe pain or difficulty urinating. Severe cases can involve larger, widespread lesions, secondary bacterial infections, lung infections, and complications like encephalitis, myocarditis, and pneumonia. Severe disease may require hospitalization, and the mortality rate for Mpox varies between 0.1% and 10%.

Swollen lymph nodes are a hallmark feature distinguishing mpox from other similar diseases. The illness typically lasts 2 to 4 weeks, and complications can include secondary infections, bronchopneumonia, sepsis, encephalitis, and corneal infection that could lead to vision loss.
Mpox Diagnosis
Diagnosis of Mpox involves clinical evaluation and laboratory testing. Polymerase chain reaction (PCR) testing of skin lesion samples is the most reliable diagnostic method.

Blood tests may also be conducted, but skin lesion samples provide the most accurate results. Early and accurate diagnosis is crucial for managing outbreaks and preventing further spread.
Mpox Prognosis
The prognosis for mpox varies. While most individuals recover within a few weeks, severe cases can lead to complications and, in rare instances, death. Vulnerable populations, such as children, pregnant women, and immunocompromised individuals, are at higher risk for severe disease. Supportive care, early detection, and vaccination can significantly improve outcomes.
W.H.O Declares Mpox a Global Health Emergency
The W.H.O. declared the Mpox outbreak a public health emergency of international concern (PHEIC) yesterday. This declaration is the highest level of alert the W.H.O. can issue, signaling the start of a coordinated international response to the outbreak.
Dr. Tedros Adhanom Ghebreyesus, the W.H.O. Director-General, emphasized the need for global collaboration, stating, “The emergence of a new clade of mpox, its rapid spread in eastern DRC, and the reporting of cases in several neighbouring countries are very worrying. On top of outbreaks of other mpox clades in DRC and other countries in Africa, it’s clear that a coordinated international response is needed to stop these outbreaks and save lives.”

Dr. Matshidiso Moeti, W.H.O Regional Director for Africa added, “Significant efforts are already underway in close collaboration with communities and governments, with our country teams working on the frontlines to help reinforce measures to curb mpox. With the growing spread of the virus, we’re scaling up further through coordinated international action to support countries bring the outbreaks to an end.” [Source: W.H.O]
Global Spread of Mpox:
The current Mpox outbreak has mainly spread to African countries neighboring DRC Congo—the outbreak’s ground zero. One case has also been reported in Sweden, the first case in Europe.
In DRC Congo, there have been over 15,600 confirmed Mpox cases, with more than 537 deaths attributed to the Mpox virus in 2024.

The outbreak has had far-reaching consequences in the Central African nation—affecting public health, economies, and social structures. In addition to the direct health impacts, the stigma associated with the disease has also led to the discrimination and social isolation of affected individuals and communities.
Transmission of Mpox: How Mpox Spreads
Person-to-person contact
: Mpox spreads through close contact with an infected person, including face-to-face, skin-to-skin, mouth-to-mouth, or mouth-to-skin contact. People carrying the virus are infectious until their lesions have crusted over, scabs have fallen off, and new skin has formed.
Environment: The virus can persist on clothing, bedding, towels, objects, and surfaces touched by an infected person. Transmission can occur if someone touches these items and then touches their eyes, nose, mouth, or mucous membranes without washing their hands.
Pregnancy and close contact: The virus can spread during pregnancy i.e., during or after birth through skin-to-skin contact, or from an infected parent to a child.
Animals to humans: Contact with infected animals, such as monkeys or terrestrial rodents, can spread the virus. Activities like hunting, skinning, trapping, or cooking animal meat can increase the risk. Eating undercooked meat from infected animals can also cause infection.

Humans to animals: In the 2022 outbreak, there were reports of the virus being identified in pet dogs, but it is unclear if these were true. The potential for spillback from humans to animals exists, so infected individuals should avoid contact with animals, including pets, livestock, and wildlife.
Sexual Transmission: Although Mpox is not classified as a sexually transmitted infection (STI), recent studies suggest that close physical contact during sexual activities, including intercourse, can facilitate the spread of the virus. This has been particularly evident in past outbreaks, where a significant proportion of cases have been linked to sexual contact.
The potential for sexual transmission highlights the need for targeted public health messaging and interventions, particularly among high-risk groups. [Source: W.H.O]
Prevention Measures for Mpox
Preventive measures for Mpox include avoiding contact with potentially infected animals, practicing good hygiene, using personal protective equipment (PPE) when caring for infected individuals, and vaccinating at-risk populations. Public health campaigns focusing on reducing risky behaviors, particularly those related to sexual transmission, are also crucial.

On a personal level, you can protect yourself by knowing the symptoms, understanding how the virus spreads, and taking appropriate actions if you suspect infection.
Avoid close contact with infected individuals, clean your hands regularly, and seek medical advice if you think you may have contracted Mpox.
If infected, isolate yourself until all lesions have healed.
In areas where animals carry the virus, avoid contact with wild animals and cook meat thoroughly before eating.
The Relationship Between Mpox and Smallpox
Mpox and smallpox are both caused by orthopoxviruses and share several clinical features, including a characteristic rash. However, mpox is generally less severe and less transmissible than smallpox.
The eradication of smallpox through a global vaccination campaign in the late 1970s provided valuable lessons for managing Mpox outbreaks. Cross-protection from the smallpox vaccine has also been a critical tool in controlling the spread of Mpox. Smallpox vaccines are usually applied as a preventive measure against Mpox.
Mpox Mutation and New Variants
One of the most concerning aspects of the current Mpox outbreak is the emergence of new variants of the virus. Genetic sequencing of samples from different regions reveals mutations that may affect the virus’s transmissibility, virulence, disease severity, and vaccine efficacy.
These mutations are believed to have arisen due to the virus’s adaptation to new hosts and environments, including urban settings with dense populations. The emergence of these variants poses a challenge for public health authorities, as they may impact the effectiveness of existing vaccines and treatments.

Continuous genomic surveillance is necessary to monitor changes in the virus and adapt public health strategies accordingly. Researchers are also exploring the potential for the virus to develop resistance to antiviral treatments, which could further complicate outbreak management. Past MPox outbreaks have shown the importance of international collaboration in tracking and responding to these variants.
Mpox Health Risks and Global Impact
Mpox poses significant health risks, both in Africa and globally. In African countries, particularly those in Central and West Africa—where Mpox is endemic—the disease has historically been a persistent public health challenge. These regions have experienced regular outbreaks due to their limited healthcare infrastructure and proximity to wildlife reserves—with animals likely harboring the virus.
The risk of Mpox spreading to non-endemic regions, in turn, has increased due to globalization, international travel, and changing human-animal interactions.

In non-endemic regions, past outbreaks have revealed vulnerabilities in global public health systems. The rapid spread of the disease to over 70 countries, including those with advanced healthcare systems—in previous outbreaks—highlights the need for robust surveillance, early detection, and rapid response mechanisms. The W.H.O’s declaration of Mpox as a public health emergency of international concern (PHEIC) is a call to action for all nations to bolster their preparedness and response capabilities.
Public Health Responses and Capacity to Manage Mpox
The public health response to the Mpox outbreak should be multifaceted, involving a combination of surveillance, public health interventions, and vaccination. Countries should ramp up their surveillance efforts to track the spread of the virus and identify cases early. Contact tracing, isolation of infected individuals, and public health campaigns will be crucial in containing the outbreak. The availability of vaccines will also be a key component of the response.

Must-Know Facts About the MPox Virus: Available Mpox Vaccines
The vaccines available for mpox, as highlighted by the W.H.O., are MVA-BN, LC16, and OrthopoxVac. These vaccines were developed to help protect against the Mpox virus in past outbreaks and will be particularly important in managing the current one.
- MVA-BN (Modified Vaccinia Ankara-Bavarian Nordic) is a third-generation vaccine designed to protect against Mpox and Smallpox.
- LC16 is another smallpox vaccine that is seen to be effective against Mpox.
- OrthopoxVac is also used to prevent Mpox and other related orthopoxvirus infections.
Who are Mpox Vaccines Recommended For?
These vaccines are primarily recommended for individuals at high risk of exposure to the Mpox virus such as:
- Healthcare workers who may come into contact with infected patients.
- Close contacts of confirmed Mpox cases, particularly those living in the same household or having close personal contact.
- Individuals in communities where transmission is ongoing, especially among high-risk groups such as men who have sex with men (MSM).
Such vaccination strategies are focused on these groups to prevent the spread of the virus and protect those most vulnerable to severe outcomes from Mpox infection. The 3 vaccines have been crucial in controlling the spread of Mpox in past outbreaks, though emerging variants of the virus could prove resistant.

Limited Vaccine Supplies
The global supply of Mpox/Smallpox vaccines is limited, and there have been challenges in ensuring equitable access, particularly in low- and middle-income countries. There is, therefore, a need for efforts to scale up production and distribution, to meet global demand.

In addition to vaccination, antiviral treatments are being explored as potential therapeutic options for Mpox. Tecovirimat—an antiviral drug initially developed for smallpox—has shown promise in treating Mpox. It was used under compassionate use protocols in some countries during the 2022-23 outbreak. Even so, more research is needed to establish its efficacy and safety.
Final Thoughts
The WHO’s declaration of Mpox as a global health emergency underscores the need for international cooperation, robust public health systems, and equitable access to vaccines and treatments. As the world grapples with this outbreak, the lessons learned from past public health emergencies—such as the COVID-19 pandemic—will be invaluable in shaping the response to Mpox.

Mpox, while less severe than smallpox, poses a significant threat due to its potential for widespread transmission and the associated health risks. The ongoing mutation of the virus and the emergence of new variants require vigilant surveillance, and adaptability in public health strategies. Through coordinated efforts, it is possible to control the spread of Mpox and minimize its impact on global health.
MPox Q&A: Summary of Critical Facts You Need to Know About Mpox
What is Mpox (Monkeypox)?
Mpox (or monkeypox) is an illness caused by the monkeypox virus. WHO now uses “mpox” as a synonym for monkeypox.
What are the symptoms/clinical manifestations of Mpox?
Initial symptoms include fever, headache, muscle aches, back pain, swollen lymph nodes, chills, and exhaustion. These symptoms are followed by a rash that often begins on the face before spreading to other parts of the body. The rash progresses through several stages—macules, papules, vesicles, pustules, and scabs—before eventually healing.
How is Mpox diagnosed?
Diagnosis involves clinical evaluation and laboratory testing. PCR testing of skin lesions is the gold standard. Blood tests and electron microscopy can also aid in the diagnosis, but skin lesion samples are most definitive.
What are the key methods of Mpox transmission?
Mpox transmission occurs through direct contact with infected animals or humans, respiratory droplets, and contaminated objects. Notably, recent outbreaks have highlighted the role of sexual transmission, particularly among men who have sex with men (MSM).
How does Mpox spread?
Mpox primarily spreads through direct contact with infected animals, humans, or contaminated materials. Key modes of transmission include:
- Animal-to-Human: Contact with bodily fluids, lesions, or respiratory droplets of infected animals, such as rodents and primates.
- Human-to-Human: Direct contact with bodily fluids, lesion material, respiratory droplets, or contaminated objects like bedding or clothing.
Who is at risk of Mpox?
People who have close contact with someone infected with Mpox are at risk, including face-to-face, skin-to-skin, mouth-to-mouth, and mouth-to-skin contact. Those in contact with contaminated objects, such as clothing and bedding, are also at risk. Health workers and those living with infected individuals should take precautions, including using personal protective equipment.
What is the prognosis for individuals infected with Mpox?
The prognosis for mpox varies. While most individuals recover within a few weeks, severe cases can lead to complications and, in rare instances, death.
What is the relationship between Mpox and sex?
Mpox can spread through close contact, including kissing, touching, oral, and penetrative vaginal or anal sex with an infected person. Individuals with multiple or new sexual partners are at higher risk. Anyone with new or unusual rashes should avoid close contact until tested for STIs and Mpox.
Are gay, bisexual, or other men who have sex with men at higher risk of contracting Mpox?
While Mpox is not limited to any specific group, during the 2022/2023 outbreak, most cases were reported among gay, bisexual, and other men who have sex with men. These individuals may be at higher risk due to the virus spreading within these social networks. However, anyone with close contact with an infected person, especially those with multiple sex partners, is at risk.
What preventive measures are recommended for Mpox?
Preventive measures include avoiding contact with potentially infected animals, practicing good hygiene, using personal protective equipment (PPE) when caring for infected individuals, and vaccinating at-risk populations.
How can I protect myself and others against Mpox?
Avoid close contact with infected individuals, clean your hands regularly, and seek medical advice if you think you have Mpox.
Can the Mpox virus mutate and new variants emerge?
The Mpox virus, like other viruses, can mutate over time, potentially leading to new variants. These mutations can affect virus transmissibility, disease severity, and vaccine efficacy.
What vaccines are available for Mpox?
The vaccines approved by W.H.O. are MVA-BN, LC16, and OrthopoxVac. [Source: W.H.O]